
We recently observed Stroke Awareness Month, so here at CIONIC, we wanted to discuss a relevant topic: walking after surviving a stroke. As you might imagine, we feel very passionately about one’s ability to walk — especially for individuals with a mobility difference precipitated by a diagnosis like a stroke. Mobility is important not only for maintaining independence, but also for empowering us all to show up for our communities, families, and friends. While walking after a stroke will likely look different than it did before, it doesn’t mean that one can’t show up with intention and attention to the world around them with maximized mobility.
Walking after a stroke: the role of rehab
If you or someone you know suffered a stroke, treatment will begin with rehabilitation. Fortunately, we live in an age where information is at our fingertips, making rehabilitation more accessible than ever before. Rehabilitation is crucial to maximizing mobility following a stroke. It is also the gateway for other benefits like assistive devices (walkers, ankle-foot orthoses and other braces, FES devices like the Cionic Neural Sleeve, etc.), home modifications, support groups, and list goes on!
During rehabilitation, as many as three different types of therapies may be included — physical therapy, occupational therapy, and speech therapy. While gait (or walking) training typically occurs in physical therapy, therapeutic techniques implemented in occupational therapy and speech therapy help to facilitate walking as well.
For example, playing games or performing activities in occupational or speech therapy that encourage engagement with both hemispheres of the brain can be very meaningful to one’s coordination (see this research article for a bit more information!).
Activities of daily living performed with an occupational therapist help to promote balance and core strength. These are both necessary building blocks for walking. Bottom line, we do many things every day that can help promote walking. And all of the therapies received can be considered precursors to increased mobility.
Pre-gait activities in the early stages of stroke rehabilitation
Physical Therapists will help to initiate “pre-gait activities.” These often include strengthening of the legs, transfer training (how you get from one place to another), balance exercises, coordination activities, core strengthening, spasticity management, prosthetics and brace fittings, and assistive device selection and fitting.
See below for a few examples of pre-gait exercises. These should be conducted under the supervision of a therapist or trainer. Once these tasks are completed or underway, gait training can begin.
Sit to Stands:
Sit to Stands are an essential functional exercise that helps with getting out of a chair, transferring, and more. If you have a Neural Sleeve, you can perform Sit to Stands in the CIONIC App with the support of the stimulation.

- Seated in a stable, firm-backed chair with arms, scoot to the edge of the seat
- Place hand(s) on the armrest
- Lean forward
- Push through the legs and arm(s) to stand
- Transfer hand(s) to assistive device
Romberg (test and exercise!):
This is a dynamic and highly modifiable exercise designed to assess challenges with balance and proprioception.

- Stand in a corner with arms down at the side or crossed over the chest
- Stand with your feet together, or slightly apart depending on balance
- The eyes can remain open or closed depending on balancing ability
- Hold the position for a predetermined amount of time or as long as possible, depending on the goal (test vs exercise)
Balloon Volleyball:
This exercise is used in therapy to challenge balance and coordination — both of which are important for walking safely!
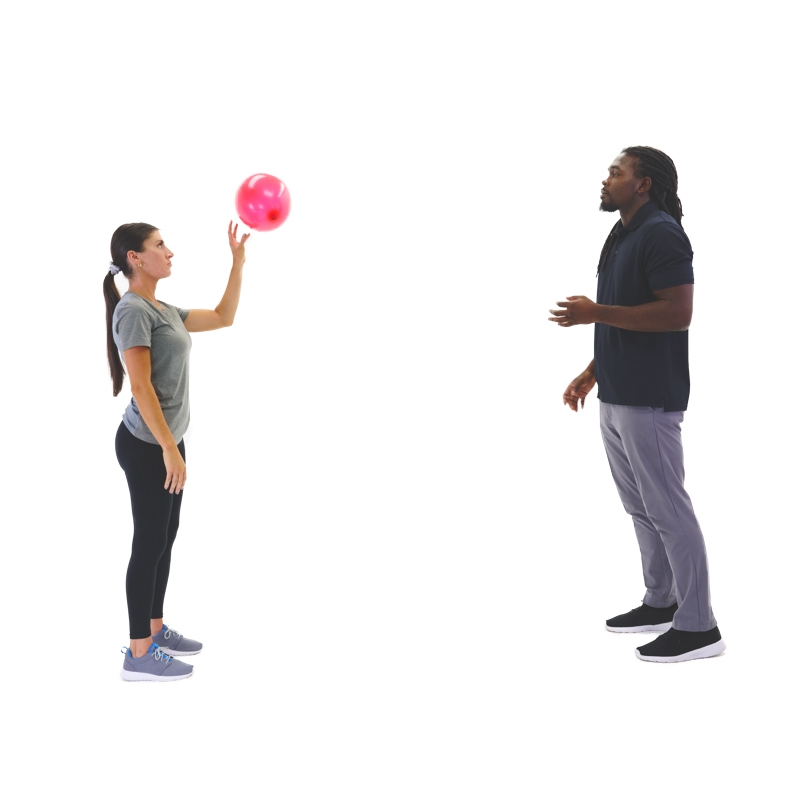
- With a gait belt and additional helper to provide stability and assistance, stand in front of a stable chair
- If relevant, your assistive device should be positioned in front, within reach
- As the therapist taps the balloon toward their patient, the patient will reach out of their base of support to challenge their balance and tap the balloon back with one or both hands
- Sit down or reach for your assistive device as needed to recover balance
Standing Marches:
This exercise helps to re-train the hemispheres of your brain by mimicking the reciprocal movement executed during walking while helping to strengthen the muscles in your legs!

Variation 1
- While holding an assistive device, shift weight toward involved/weaker side and lift opposite leg
- Repeat to focus on weight shifting, with assistance stabilizing the weight-bearing side as needed
- A low box can be included to place the lifted foot on to mimic a “step-up.” If you have a Neural Sleeve and can safely perform standing exercises, the new Step Ups functional exercise protocol will help with this!
Variation 2
- While holding an assistive device, shift weight toward involved/weaker side and lift opposite leg
- Alternate and shift weight toward uninvolved/stronger side, lift opposite leg
- Even if the foot is not lifted very high, this is a great activity to focus on. It can be done with assistance lifting the leg and foot as needed
Gait training to promote walking after a stroke
Gait training is actually much less complex — though still challenging — than pre-gait training because the main activity is walking! Tasks, distance, assistive devices (such as hemi-walkers and quad canes), and assist level will vary greatly.
Depending on the severity, not everyone will be able to walk again after having a stroke. In these cases, therapists will work with their patients to maximize mobility and increase independence.
The goal of gait training is to enable someone to walk as much as possible, with the least cumbersome assistive device and braces possible, while still being safe. A question we often receive at CIONIC is: “Will I be able to stop using my walker/cane?” And the answer is always, “That is up to you and your therapist because we want you to be safe”.
A therapist will most likely place a belt around their patient to hold onto to help provide stability and security. They may decide to schedule therapy during a time when another therapist or aide is available to assist in keeping the patient safe by following with a wheelchair, helping to advance a foot, stabilizing an arm on an assistive device, or — with patients with higher levels of mobility — challenging their balance while they are walking.
The therapists will set short-term and long-term goals for each patient and create a treatment plan to reach those goals. A patient’s input is very valuable here as the entire team wants to focus on what is important to each patient and what their goals are.
Challenges of relearning how to walk
Relearning how to walk after a stroke is not easy. It requires patience, determination, and resilience. There may be moments of frustration and setbacks along the way, but it’s essential to stay focused on the goal of maximizing mobility.
Challenges individuals may face during walking rehabilitation include:
- Muscle weakness and stiffness: Weakness in the affected limbs and stiffness in the muscles can make it difficult to initiate and sustain movement.
- Balance and coordination deficits: Impaired balance and coordination increase the risk of falls and may require intensive training to address.
- Fear of falling: A fear of falling can hinder progress and lead to decreased confidence in walking independently.
- Fatigue: Stroke survivors often experience fatigue, which can impact their ability to participate fully in rehabilitation activities.
- Cognitive impairments: Some individuals may struggle with attention, memory, or problem-solving skills. This can affect their ability to follow instructions and engage in therapy.
Despite these challenges, significant progress is possible. With the support of rehabilitation professionals, family members, and friends, individuals can overcome obstacles and make significant strides in their recovery journey.
Additional treatment options and assistive devices for stroke survivors
Treatment plans for someone who has had a stroke might also include modalities like functional electrical stimulation (FES). FES can help activate and educate the muscles weakened by a stroke, alongside strength, balance, and gait training.
The Cionic Neural Sleeve is an assist device for individuals who have had a stroke. It uses functional electrical stimulation during the gait cycle to promote strength, neuroplasticity, neuromuscular re-education, sequencing of muscle contractions, and cueing for the brain all while the user is walking. This technology is particularly beneficial for those who have incurred foot drop from a stroke or other lower extremity weakness that impacts their walking ability.
If you are interested in learning more about the Cionic Neural Sleeve, head to cionic.com/assessment to answer a few questions. Please be ready with an assistant and a tape measure to provide measurements. And don’t hesitate to reach out to us at support@cionic.com with any questions you might have! Our team is full of highly qualified mobility experts waiting to assist you.





