
I’m Jan. I have a life-long condition of cerebral palsy. Here is my story.
I was born three months prematurely in July 1951. I was told all my life I was something of a miracle baby. I measured 10 inches long and weighed about 24 ounces. (I love to bake, so looking at six sticks of butter shocks me from time to time.) Too tiny to survive, yet close to 72 years later, I have.
It was touch and go in those early days and weeks. My young parents, and two year old sister, really wanted me at home with them. I lived in the hospital neonatal intensive care unit for over two months until I weighed an impressive 5 pounds.
Early on, my parents realized I wasn’t reaching the same physical benchmarks my sister had at the same age. The doctors and other professionals dismissed their concerns. “Every baby comes with their own schedule” was a common refrain.
Language and vocabulary was not difficult. In fact, I was known for being wordy! I often answered in complete sentences rather than a word or two, as many children do. That hasn’t changed. So, consider yourselves warned. This might be TL;DR for some. For the rest, make yourselves comfortable.
A diagnosis of cerebral palsy was determined
I was three and just learning to walk with difficulty when a diagnosis of cerebral palsy was determined. My gait was pretty classic for CP. Shortened heel cords meant I walked on my toes. Very tight adductor muscles turned my feet in. Balance was particularly tricky since I was constantly on tiptoe, poised to tip forward. Unpredictable spasticity caused issues. Everything seemed to tighten up just when I needed the opposite effect. (To this day, that still happens, particularly under stress.) As a toddler, I fell frequently. My movement of choice was often to commando crawl.
At three, I started physical therapy

I started physical therapy at Stanford Medical Center, Palo Alto, California, shortly after my third birthday. We were fortunate to live in the Bay Area, just a few miles from Stanford’s extensive physical therapy department and teaching hospital.
From the time I was three until I was 12, I had hundreds and hundreds of sessions with a myriad of therapists and students. Some of those tips and tricks are fully embedded in my subconscious. I am constantly evaluating my mobility and gait to this day. “Chin up.” “Tummy in.” “Pelvic tilt.” “Heel first, then toe.” And so it goes.
Braces, orthopedic shoes, surgeries, and more
In those early years I wore braces. Cumbersome frames with straps or pipes provided an exoskeleton to help me rotate my feet out, rather than allowing them to turn in naturally. I wore braces at night for a time, too. More about that later.
The braces required heavy orthopedic shoes to accommodate special hardware. Shoes that needed to be painted with white nurse’s shoe polish nightly to cover up all the rough and tumble scraping and scratching from constant foot drop during the day. It was the 1950s after all. Little girls wore dresses and saddle shoes to school. Mine were never quite real saddle shoes, and certainly never popular.
But they were funny! My parents taught me to lean on humor to cope with tricky situations. When the hinges of my braces tore holes in the sides of my underwear, my mother and I would laugh and say, “Look they are air-conditioned!” Hanging up my contraption of long black pipes with big orthopedic shoes on a hook in my closet, reminded me of Popeye’s wife’s physique. That set of braces became “Olive Oyl.” Olive Oyl served me well.
Along with continuous therapy appointments, I had surgeries as a child to try and mitigate my condition. When I was 9, I had both gastrocnemius muscles lengthened at the same time. This meant both legs were in casts for several weeks in winter. Fortunately, there were heels on the casts so I could get around with help.
As a treat, we went to the drive-in movie in our station wagon, since I couldn’t sit in a movie theater. At intermission between cartoons and the main feature, my mom and sister helped me walk to the restroom. Two teen boys looked at me, smiled and said, “Someone’s been skiing!” I was thrilled. Those boys thought I could ski! It was February and I fit right in! Ahh, camouflage. My favorite.
All of my sessions with physical therapy allowed me to see people with a range of ability. I didn’t use crutches or a walker. I knew how fortunate I was to be able to walk with and without assistive devices, and not be in a chair. I attended regular education classes. I know now that my parents had to advocate strongly for me to do that. My mobility difference confused children, but it also baffled some teachers. I was fortunate to be placed with (mostly) compassionate teachers and classmates.
Cerebral palsy affects both of my legs, but my left leg is markedly more involved. When I was 11, I had an operation that was quite new in 1963. A left hip osteotomy. This surgery was meant to be a last resort to correct my gait. My left leg was repositioned, rotated more firmly out, securing my hip placement with four pins.
After extensive physical therapy, the operation was deemed a success. My physical therapist and orthopedic surgeon basically said, “There’s not much more that we can do. Stay flexible and work hard on your mobility on your own.” Twelve-year-old me was ecstatic! No more braces! No more hospitals! No more therapy! That was true for a long time. I was able to walk independently of any devices from the age of 12 until my late twenties.
My gait, however, has remained compromised. I have never run, unless you count jogging in water aerobics. The only two-wheeled bike I ride is either stationary, or the back seat on a tandem.
In middle school and high school, I earned PE credits by keeping score, or tidying the locker room. I still enjoy lots of sports as an observer, but never a participant.
Early adulthood with cerebral palsy
From the age of 8, I knew I wanted to be an elementary school teacher. I was a freshman majoring in elementary education in college in Boston when I met Alan. He was from England, in the United States as a business intern. Love bloomed. When his year-long internship ended, I returned to England with him. We were married in his hometown of Liverpool in 1970. I was 19. I completed my teacher training at Liverpool University and taught in the English school system until we returned to the States six years later.
Those were wonderful, challenging years. I loved my job with a passion. I walked everywhere. I didn’t drive. (I wasn’t interested in learning how to drive on the left-hand side of the road.) I rode double-decker buses, and managed to get lost and found frequently.
The English people I met were immensely welcoming. Not much was made of my mobility difference. Occasionally someone might inquire if I had hurt my foot. I accommodated my tightened heel cords by wearing short, stacked-heeled shoes that were in fashion.
I often got the toes of my shoes capped to protect them from excessive wear due to my foot drop. I had a wicker basket on wheels (shopping trolley in Brit speak) that allowed me to cart all manner of things beyond groceries. It also provided a certain level of support over cobblestones and difficult terrain. Camouflage in action!
Returning to California and becoming a mom
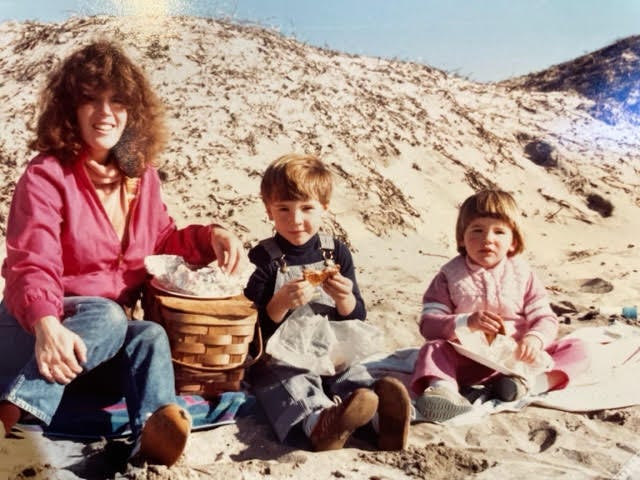
Returning to California in 1976, I worked in preschools and as a substitute teacher until our son was born in 1979. Since I still didn’t drive, I rode an adult tricycle all over our small community of Half Moon Bay. Being pregnant and recovering from a cesarean section wasn’t without issues, but pushing a stroller with a healthy baby was easy!
I couldn’t go everywhere and do everything on my trike or with the stroller though, so I learned to drive when our son was one. Our daughter was born (another c-section) a year later, just before I turned 30 in 1981. Both pregnancies (and surgeries) aggravated my scoliosis and compromised my gait further. I used a walking cane when I was pregnant. Alan was an amazing hands-on dad. Together we managed pretty well. I would fall from time to time (I have mastered a ‘tuck and roll’), but miraculously the children were always safe. They thrived. We all did!
Falls escalated and something needed to change
Time passed. I needed surgery for a bunion on my right foot, the alleged ‘good’ leg. The bunionectomy went badly awry. Without a stroller to push (the children were about seven and five) my foot drop was pronounced. I had back pain and the falls escalated. Something had to change.
I was 35. I knew I needed to renew some kind of formal support to manage my CP. I reached out to my former physical therapist and orthopedic surgeon, both retired. They recommended more physical therapy and a visit to a physiatrist whose office was right back where I’d had surgeries as a child. I wasn’t happy about it. I was annoyed and frightened. How much worse would my condition get? How quickly? What about the kids?
My physiatrist was very kind. No, there weren’t any new developments for treatment of CP. He was very apologetic. All he could recommend was, surprise! More PT. Oh, and a disabled person’s parking placard. Alan and I followed up on both. It was a difficult time for me. I felt l had failed somehow. No camouflage. A label.
A good physical therapist treats the whole person, not just the prominent ailment. There has to be a good match. Cerebral palsy is not a sports injury. The exercise routines will not repair the condition. They relieve some discomfort. They strengthen. They help one cope within a skiIl set.
I have been very fortunate. I have worked with many skilled therapists in my life. Two in my adult life have been exceptional. Every single one has coached my work in strength, balance, and gait, always gait. I carry pieces of advice from each of them. Voices in my head with every step. It can get very noisy!
Working hard to stay mobile as I’ve aged
Cerebral palsy isn’t a degenerative condition, but birthdays are. Working hard to stay mobile has been a constant theme for me as I have aged. Bike rides, water aerobics, walking hand in hand with Alan or the kids. All of that, along with formal PT when we could get insurance to cover costs, helped. I used exercise equipment at home. I hired people to help at home with my exercise routines from time to time, too. It’s a lot easier to stay on track when someone else is working with you. Exercising is just so daily!
Back to teaching
When our kids were eight and ten, I went back to teaching first grade and kindergarten in elementary school. Once again, I loved my job. It seemed like something was wrong with the clock in my classroom. Time went faster there than anywhere else!
Parents and students were naturally curious about my condition. I clearly walked differently. Some parents worried that their children would not be safe with me. What if there was an emergency? Would I get the children out quickly enough?
I was fortunate to work with colleagues and administrators who supported my position in the classroom. Every year, I took time during the first two days of school to discuss “my funny old legs.” I explained to the children the part of my brain that made my legs work was damaged when I was born. We agreed that I was there to help them, and they could be there to help me. We were a team.
Clearly, that message went home with one student when his mom called me to say that her six-year-old son had come home on the second day of school with “GREAT NEWS! Guess what?! My teacher’s legs aren’t connected to her brain!” I couldn’t have put it better myself!
Experiencing distinct decline in my 40s and 50s
In the nineties, when I was in my 40s, I experienced a distinct decline in my ability to cross an open space confidently without support. Time to find another physical therapist. Buckle down and work harder. Still teaching, I compensated by using a market basket to carry teaching materials, but also provide additional support. No cobblestones here! I designated a student in my classroom each year to be a “steady walker” with me when we traveled around the campus. It became a popular role!
In 1998, when I was 47, I was diagnosed with breast cancer. A double mastectomy changed my gait dramatically. Though I recovered well, and have remained healthy, ensuing surgeries took a toll on my body. I was forced to reckon with the scope of my mobility difference. The market basket was exchanged for a three-wheeled walker whenever I was out in the world alone. In the classroom, the kids called it my ‘scooter.’
I was 54 in 2005, when at the urging of my first outstanding physical therapist, Eddie, I returned to visit the physiatrist I had met 19 years before.
New drugs to mitigate CP
Now there were drugs to try to mitigate CP. Baclofen and Botox. Eddie told me working with me was like lifting marble. “I can only imagine what it’s like for you on the inside,” he said.
My physiatrist prescribed Baclofen which offered relief of my spasticity. I had no idea of the discomfort I was in until it went away! I tolerate Baclofen well, and I still take a low dose daily. He also administered Botox. I had Botox shots to my adductors every 12 weeks for five years. I found that more difficult to manage, but it helped keep me mobile.
The fall of a lifetime
Shortly before I turned 60 in 2011, I had the fall of a lifetime, while using my walker. That truly frightened me. Now what? What was next? I used the summer to recover and research options. My heel cords were too tight once more. The efficacy of Botox had run out. Once again, surgical treatment, very similar to the surgeries I had when I was nine, was required.
I retired from teaching in 2012 and had surgery on both legs simultaneously again. Once again, I was in double casts, non-weight bearing this time. My Achilles tendon was lengthened on my left leg. Fascia was released around my gastrocnemius muscle on my right leg. Even with lots of gait training after these surgeries, I had to rely on a quad cane for support indoors and out. I have used one ever since.
I still named my devices. Between ‘The Stick’ (cane) and ‘The Harley’ (walker), I got around well enough. It took a lot of work. I am strong, but my spasticity is often stronger. When it’s hard to move, you don’t move much. And then, it’s harder to move. I tried to stay active using exercise machines and in-home therapy support, but my range and stamina were dwindling.
In 2014, I began working with my second amazing physical therapist, Adelita. We tried all kinds of things. Bands, machines, and even an exoskeleton called Kickstart that worked on muscle memory for a more normalized gait. For the first time, I experienced what able-bodied people do when walking. Kickstart taught me I needed to lift my feet as if I was marching in snow!
Between the voices in my head, moving marble, and marching in snow with every step, walking was very challenging. I perspired a lot over short distances, even with the Harley. It was hard to walk and hold a conversation. I was frequently breathless. My easiest and most favorite place to walk was in a pool!
Night braces… again
A formal digital gait analysis at Stanford in 2017 spelled out very clearly the depth and breadth of my mobility difference. A whole new regime of exercises was prescribed to support my aging spine. New and improved leg work, and a four-wheeled walker was recommended. I was advised to wear night splints to help control my dorsiflexion. What goes around comes around! Night braces again at the age of 66, just like being three years old. I wear them still.
The pandemic didn’t help. Sheltering in place curtailed all manner of activities, including formal physical therapy and help with exercise at home. I worked to stay active on my recumbent elliptical bike daily. Not inspiring, but useful. I walked less and less.
Participating in a mobility trail for adults with CP
In the spring of 2021, Adelita texted me. Was I interested in participating in a mobility trial? Yes! She was attending a conference via Zoom. Jeremiah Robison and his team were presenting a new concept, Cionic’s Neural Sleeve. Bionic clothing? With an app? Adaptive algorithms programmed to take over and stimulate my leg muscles when my brain does not? Perhaps my legs could be connected to my brain!
I contacted Cionic and told some of my mobility story. I was concerned I might not qualify. The trial seemed to be limited to people up to age 70. I would be 70 in July. Was I now too old to try this amazing device created with cerebral palsy in mind? Fortunately, the answer was “No.”
Alan and I went to the home office of Cionic in San Francisco. In a new setting, dealing with my condition, I often experience ‘performance anxiety.’ I needn’t have worried. The entire team at Cionic was welcoming, supportive, and kind. Their energy and commitment to this new endeavor was palpable.
My gait was evaluated and tracked electronically. The sleeve, still in prototype form, was fascinating. This garment could fit under clothing and resembled a legging. Embedded electrodes would stimulate my muscles and promote a more normalized gait, designed for me, using an app on my phone. Wow. There is nothing like the elixir of hope.
All good things take time. That initial evaluation was in May 2021. I returned to Cionic to receive a prototype sleeve in March 2022. I felt support within 90 minutes of my first fitting! I have worn it nearly daily ever since, with truly remarkable success. A custom-made sleeve for my left leg is in the pipeline. A second sleeve for my right leg is in the works.
There is a learning curve wearing the Neural Sleeve. From the beginning with Cionic, everyone on the team has been and remains eminently helpful and supportive. Alan and I are fortunate to be close to Cionic’s headquarters here in the Bay Area, so we can make in-person visits.
Additionally, team members are as close as a text, phone call, or FaceTime away. Each of the team members is eager to resolve any issue with remarkable empathy and expertise.
Navigating the app takes time to understand. Finding the right level of stimulus in the settings to support my gait has required trial and error. As far as wearing the sleeve from the standpoint of fashion, it’s a personal choice. I prefer to wear dresses and boots or long skirts over my sleeve. They are easy and comfortable — and yes, happily for me, they provide camouflage.

The Cionic Neural Sleeve: the best device I’ve ever worn
The Neural Sleeve is, without exception, the best device I have ever worn to help me manage my CP. The exercise routine included in the app targets each of the four muscle groups required for walking. It’s easy to follow and has made me stronger.
The benefits of the neural sleeve are phenomenal. The sleeve has changed the trajectory of my mobility. I honestly feel as though wearing the sleeve has helped me turn back time. What follows is a list of experiences made possible for me wearing Cionic’s Neural Sleeve:
- My foot drop has been alleviated remarkably.
- I now transition easily over varied terrain, pavement, gravel, lawn, wood chips, bricks.
- Places that have been off-limits for well over 15 years are accessible once more.
- I walk new places with greater confidence.
- I look up and hold a conversation while walking.
- I rarely fall.
- Walking is easier. I am not ‘moving marble’ anymore!
- My stamina has increased exponentially.
- I have more energy for everyday activities.
- I don’t perspire the way I used to while walking.
- My range has increased.
- I stand up straighter now.
- My chronic back pain has lessened substantially.
- I can walk a greater distance and for a longer period.
- There is carryover strength and balance when I take the sleeve off.
In the middle of a medical miracle
I honestly feel as though I’m in the middle of a medical miracle. I have lived long enough to benefit from life-changing technology. Wearing the sleeve, I still use my stick at home. I use the Harley if I am out in the world alone. Using a walker is a solitary activity. The Neural Sleeve has granted me a closeness with special people I thought was gone for good. Thanks to Cionic, I can walk arm in arm with my loved ones once more.
That, to me, is priceless.
This is a user story from a Cionic customer, who has not been compensated to share their story. Individual results and experiences may vary. Consult with your doctor on treatment decisions.





